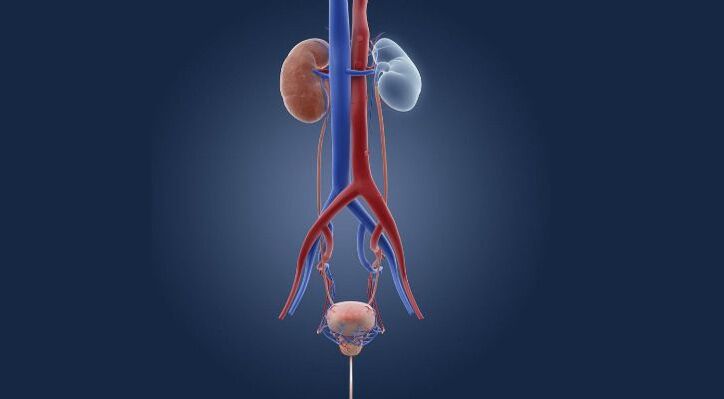
Cystitis is an inflammation of the bladder. This organ is intended for the accumulation and excretion of urine, but if the lining of the organ is damaged, its function suffers and the person begins to experience unpleasant symptoms. In most cases, the pathology affects only the mucous membrane, but sometimes the inflammatory process extends to the muscle tissue. Interstitial cystitis is the most difficult to treat.
The disease mainly affects women, which is related to the anatomical features of the urethra. Inflammation in men occurs rarely, usually acting as a comorbidity in the context of chronic prostatitis.
Symptoms
The signs of cystitis are quite obvious and it is difficult not to notice them. As a rule, the disease begins acutely, so patients pay attention to the obvious discomfort in the urinary system. Among the manifestations of pathology note:
- frequent urge to urinate.
- feeling of incomplete urination;
- cramps and pain when urinating.
- increase in body temperature;
- the appearance of an admixture of blood in the urine.
- cloudy urine (due to the presence of pus);
- nausea, drawing pains as during menses.
Despite the characteristic symptoms, the disease can present different manifestations. Hematuria is not always present, but the pain on tension may feel like only mild discomfort. In any case, if signs of pathology appear, it is necessary to consult a doctor to make a diagnosis as early as possible. The disease in the acute phase at an early stage is better treated, but the chronic form takes longer to fight.
Forms and types of chronic cystitis
By the nature of the inflammatory process, cystitis is acute and chronic. Depending on the source of growth, the disease can be primary (independent disease) or secondary (inflammation spreads from neighboring areas, such as the kidney).
According to the area of damage to the mucous membrane of the bladder, cystitis occurs:
- total (general);
- focal.
The following clinical forms of cystitis are distinguished:
- catarrhal - non-purulent inflammation of the bladder mucosa.
- inflammatory - purulent damage of the submucosal layer.
- granulomatous - accompanied by rashes on the mucous membrane.
- hemorrhagic, which is characterized by the release of blood in the urine.
- interstitial cystitis - inflammation spreads to all layers of the organ.
A number of rare forms are also distinguished: ulcerative, cystic, gangrenous cystitis.
All the variety of inflammatory diseases of the bladder is combined into two large groups:
- specific cystitis, caused by sexually transmitted pathogens: gonococci, ureaplasma, chlamydia.
- non-specific cystitis - develop due to opportunistic flora, the representatives of which under normal conditions do not lead to diseases (for example, E. coli).
Finally, non-infectious cystitis is combined in a separate group. They can appear under the influence of allergic factors, radiation, traumatic, thermal effects, parasite toxins.
Causes of cystitis

In most cases, damage to the bladder and the development of the inflammatory process is associated with the penetration of infection, however, cystitis can be toxic and allergic. When an infection enters, the disease is spread in several ways:
- ascending - from the urethra through the urethra - affects the bladder.
- descending - in this case, the infection occurs due to inflammation of the kidneys, through the ureters, reaches the bladder.
- lymphogenic - with the flow of lymph through the pelvic organs in the presence of genital lesions.
- hematogenous - the infection enters with the bloodstream, but this route of spread is the rarest.
- direct - if an abscess breaks inside the bladder and the pathogenic microflora penetrates directly into the bladder cavity, it can also be during the catheterization of an organ, infection during surgery.
Most of the time, E. coli causes cystitis. It occurs in 80-95% of cases of uncomplicated pathology. This bacterium is normally found in the rectum, but when it enters the urethra, it causes an inflammatory process. Enterobacteriaceae, staphylococci, fungi, sexually transmitted infections can also cause the disease. It usually precedes the onset of symptoms of vaginitis or bacterial vaginosis, and you can also notice the symptoms of the disease within a day after intercourse (postcoital cystitis).
Factors that contribute to the development of cystitis
The body with good immunity can cope with the presence of pathogenic microflora, so the symptoms of cystitis in the patient will not appear. But when exposed to certain factors, it manifests itself:
- injury to the mucous membrane of the bladder.
- circulatory disorders of the pelvic organs.
- hypothermia;
- the presence of other foci in the body, such as kidney infections.
- reduction of the body's defenses.
- inflammatory diseases of the genital organs.
- lack of vitamins and minerals in the body.
- hormonal imbalance;
- poor hygiene, wearing synthetic underwear.
- stress and overwork;
- delayed bladder emptying.
In the presence of these factors, cystitis will progress rapidly and the chronic pathology will pass into the relapse stage. Therefore, in order to avoid relapses, it is necessary to exclude the influence of causative factors on the body.
Causes of the transition of acute inflammation to the chronic phase
The inflammatory process in the bladder can occur due to various pathogenic factors. Most often they are bacteria, but there are cystitis and viral, fungal etiology. If the acute form of the disease is diagnosed in time, the correct treatment of cystitis is prescribed and the patient follows all the doctor's recommendations, then the pathological process can be completely eliminated and recovery will come.
But often women postpone visiting a doctor, try to treat cystitis on their own, hoping that everything will go away by itself. As a result, valuable time is wasted. Microorganisms actively multiply, the intensity of inflammation increases. Having completely "settled" in the bladder, the germs will not leave their places so easily. The inflammation becomes chronic.
It is also common for a specialist to prescribe treatment for cystitis, the patient starts taking medication and stops the treatment on her own the moment she feels relief. As a result, the pathogens are not completely destroyed and the survivors are divided - chronic cystitis is formed, which is resistant to antibiotic treatment.
Finally, the following conditions contribute to the development of chronic cystitis:
- general reduction of immune defense, hypothermia.
- hormonal changes (pregnancy, menopause);
- neglecting the rules of personal hygiene;
- gynecological diseases;
- chronic diseases of other organs and systems: diabetes mellitus, malignant tumors.
Signs of chronic cystitis
In the medical community today, the very term "chronic cystitis" is outdated. It is used "the old way", for better communication with patients. A subdued inflammatory process in the bladder is called recurrent cystitis. The main symptom is the development of 2 or more exacerbations within six months or 3 episodes per year.
The period of exacerbation is accompanied by characteristic symptoms:
- frequent urination;
- pain, burning, pain during urination.
- night calls;
- feeling of incomplete evacuation, pain in the lower abdomen.
The exacerbation of the disease may be accompanied by a moderate increase in body temperature, the appearance of blood in the urine, its turbidity.
During the period of remission, the symptoms can be completely normalized. But more often, patients suffer from discomfort during urination and periodic moderate pain for years.
The most serious consequence of recurrent cystitis is the development of resistance (resistance) of pathogens to antibacterial drugs and the subsequent degeneration of the bladder mucosa. The mucosal epithelium undergoes striated deformation or is replaced by a stratified squamous one. At this stage, chronic cystitis can no longer be treated with antibiotic therapy alone. It is necessary to carry out special medical procedures.
Acute and chronic cystitis: therapeutic approaches
The treatment of acute and chronic forms of pathology is different. Usually, acute cystitis is much easier to treat, because the pathology is caused by microorganisms, against which the doctor will prescribe a course of antibiotic treatment. Antibacterial drugs are quite different. They quickly help to stop an attack of the disease, and the systematic use of funds will lead to a complete cure for cystitis. Preparations based on fosfomycin perfectly cope with inflammation.
Chronic inflammation is more difficult to treat because it is complicated by other disorders. Complex treatment of long-term developing cystitis is carried out using various groups of drugs. Antibiotics remain top-of-mind, but the doctor will also prescribe anti-inflammatory drugs, vitamins, and remedial medications. As a prevention of infections and to consolidate the effect of the treatment, the patient is prescribed herbal medicines, physiotherapy courses.
cystitis in women
Most often, cystitis in women is accompanied by exacerbations of chronic inflammation, therefore, according to statistics, every second patient consults a doctor with a recurrent disease twice a year.
This speaks not so much about the difficulties in treating the disease, but about the need to carefully follow the doctor's prescriptions and eliminate the factors that cause the disease.
cystitis after intercourse
Postsynovial cystitis in women is caused by abnormalities of the genitourinary system. When it shifts down and into the external opening of the urethra, it becomes more susceptible to the penetration of pathogenic microflora. Also, the culprit of cystitis is a very mobile urethra, which is easily displaced when the penis is rubbed. In this case, the mucous membrane is easily irritated and pathogenic microorganisms penetrate the opening of the urethra. The symptoms and treatment of this form of pathology are interrelated, so doctors approach the problem individually in each clinical case.
Also, the causes of cystitis are the alternation of anal sex with vaginal sex, which is absolutely impossible to do, because the microflora of the rectum enters directly into the vagina and the adjacent urethra. A factor in the development of bacterial infections is the introduction of microbes by hand, insufficient secretion of vaginal mucus, which causes microcracks.
The symptoms of postconjunctival inflammation do not differ, but the patient can notice their appearance immediately in connection with sexual intercourse - usually the discomfort appears already in the first 12 hours.
The treatment of post-synovial cystitis is individual, since first it is necessary to determine the cause of the disease and to precisely direct the treatment. With an abnormality of the urethra, the doctor will suggest plastic surgery, as a result of which the problem will disappear. Both surgery and hyaluronic acid injections are possible. If an STD infection occurs during an intimate relationship, then antibacterial drugs will be required, followed by restoration of the vaginal microflora.
What does blood in urine mean?
The appearance of blood in the urine indicates the development of acute hemorrhagic cystitis. It does not appear at the end, but accompanies the entire process of urination. The presence of erythrocytes gives the pink color to the urine. Also, urine can be "meat" colored, i. e. have a brown color with the presence of mucous strands, threads or brown flakes.
Usually, when you urinate with blood, there is severe pain, pain in the bladder and pulling sensations in the lower back. The appearance of blood in the urine is a mandatory reason to visit a doctor.
Cystitis during menstruation
In some women, an exacerbation of cystitis occurs against the background of hormonal changes during menstruation. During menstruation, the pelvic organs are more susceptible to infection, so the following can cause the disease:
- inflammatory diseases of the female genital organs.
- hormonal fluctuations;
- allergic reaction to personal hygiene products.
- reduction of the body's defenses.
- non-compliance with personal hygiene;
- non-specific infections, fungal infections, STDs.
Under the influence of these factors, the pathogen enters the urethra and urethra, causing inflammation. Usually, an exacerbation of the disease occurs during ovulation, as well as 1-2 days before the onset of menstruation. Vaginal secretions become an excellent breeding ground for pathogenic microflora. The symptoms of cystitis during menstruation are typical, but they are complicated by characteristic manifestations during menstruation - pains and pulling pains in the lower abdomen.
The doctor can identify the cause of the pathology after collecting a history and studying the results of laboratory diagnostics. The treatment regimen is standard, but simultaneous treatment of gynecological pathologies may be required if genital infections are diagnosed. It is important to observe personal hygiene, strengthen the immune system.
Pregnancy and cystitis

According to the results of studies, doctors found that asymptomatic bacteriuria is detected even before pregnancy, therefore, during the period of pregnancy the disease manifests itself. The reasons for this are:
- changes in the hormonal background and the ratio of progesterone and estrogen in the body of the expectant mother.
- violations of urodynamics as the size of the uterus increases.
- weakening of the connective apparatus, greater mobility of the organ, but a decrease in peristalsis and its tone.
- expansion of the renal pelvis due to increased blood circulation in the pelvis.
The latent course of the pathology complicates early diagnosis. Treatment of cystitis during pregnancy is possible even with the use of antibiotics. The doctor will prescribe the names of the drugs and the doses of the drugs that are safe for the fetus.
Diagnostic methods
The symptoms of cystitis are very characteristic, but the doctor will prescribe a series of tests to finally discover the causative factor of the pathology and determine the nature of the course of the disease. The specialist will collect a history, analyze the patient's complaints and conduct an external examination with palpation of the bladder belt. The following diagnostic methods are used:
- ultrasound - using ultrasound, you can determine the degree of the inflammatory process, its prevalence, as well as assess the state of the urinary system, genitals.
- cystoscopy - examination of the organ using an endoscope, which allows you to assess the condition of the bladder mucosa.
- cystography - examination of the bladder using contrast.
In women, treatment should begin with the definition of the pathogen. A set of laboratory tests is mandatory: general urinalysis, Nechiporenko analysis, bacteriological culture, tissue biopsy, polymerase chain reaction (for a more accurate determination of the pathogen). To assess the degree of the inflammatory process, doctors can send a blood test. If there are suspicions of inflammatory pathologies of the female genital organs, an examination by a gynecologist and the delivery of the tests prescribed by him may be required.
Methods of Treatment
In inflammatory diseases of the organ, doctors resort to therapeutic and surgical methods of treating the pathology. In most cases, it is possible to get rid of the disease with a properly formulated drug treatment with the addition of physiotherapy.
Drug therapy includes a combination of different groups of effective drugs, depending on the nature of the disease. The patient may be given:
- anti-inflammatory drugs - serve to relieve swelling of the mucous membrane and eliminate pain, the inflammatory process is reduced.
- antispasmodic - used to relieve pain symptoms, effectively eliminate bladder spasms.
- antibacterial therapy - a group of drugs that act directly on the causative agent of the pathology.
- antifungal drugs - recommended if cystitis is caused by a fungus or complicated by it (for example, with a combined course of bacterial-fungal infection).
- herbal preparations - drugs in tablets and other forms that have antimicrobial and anti-inflammatory properties.
In some cases, doctors prescribe instillation of drugs to the patient instead of oral administration. Bladder lavage is performed at the clinic. With the help of a special catheter, the desired concentration of the drug is administered, which cannot be achieved in other ways. Before the procedure, the patient must empty himself, so that the drug affects the mucous membrane for as long as possible.
Surgical treatment is used only in rare cases, when the inflammatory process has caused anatomical changes or in severe recurrent infections. In this case, laser correction is performed. For example, in post-cloud cystitis, for many women, the only treatment option is distal urethral transfer.
Nutrition in the treatment of cystitis

It is imperative to follow a diet, since spicy and salty foods contribute to the appearance of ulcers on the mucous membrane. Other products are irritants that interfere with recovery:
- foods high in sugar.
- citrus, sour, fermented foods.
- seasonings;
- tomatoes and all tomato dishes, additives (ketchup, sauces, adjika).
- soy sauce and vinegar;
- nuts and chocolate.
To speed up recovery, the patient is advised a light and nutritious diet. It is necessary to exclude fried, smoked meats, marinades, fatty foods. It is best to steam, cook or boil. Eliminate all foods that can cause allergies.
An attack of cystitis may also be caused by heavy food, in which the patient suffers from constipation. With the stagnation of fecal masses, intestinal peristalsis worsens, stagnation occurs in the bladder, as a result of which the mucosa is irritated again. Due to the high protein content you should not eat a lot of meat, fish, beans, cheese. Replace them with foods rich in plant fiber - vegetables and permitted fruits.
During treatment, try to eat at home, cook for yourself and do not include new foods or dishes in the menu. Keep in mind that the diet completely excludes alcoholic beverages and also limit coffee and tea. Juices, decoctions and infusions of herbs, fruit drinks and compotes will be useful. It is better to replace ordinary water with slightly alkaline mineral water.
Physiotherapy
Among the methods of treating the disease, physiotherapy is widely used. As a rule, it is recommended in the recovery stage, when the acute inflammation of the bladder has been removed and there has been a positive trend towards recovery. Physiotherapy is also effective for submucous localization of the causative agent of the pathology, when antibacterial drugs do not have the appropriate effect. Physiotherapy is used:
- phonophoresis?
- electrophoresis?
- magnetotherapy?
- UHF?
- modulated currents.
The session does not last long, however, a course of 10-15 procedures is required to achieve the result. The powerful treatment of cystitis in combined ways will help you get rid of the disease completely.
Question answer
How long does cystitis last?
The duration of cystitis depends on the form of the pathology. Acute lasts 7-10 days, after which, with appropriate treatment, recovery occurs, but the chronic form of the disease can last several months, reminding itself of periods of exacerbation.
Is it possible to visit a bath or a hot shower with cystitis?
A hot shower or bath really helps to relieve spasm and pain, however, these thermal effects are contraindicated in inflammation of the bladder, as this contributes to the exacerbation of the inflammatory process.
Which doctor should I contact and what tests should I submit?
Women with suspected cystitis should contact a general practitioner, men - a urologist. If necessary, the patient can be referred for examination to a gynecologist. Tests - urinalysis, blood test and ultrasound or cystoscopy.
How does age affect the course of the disease?
Most often, cystitis occurs in women aged 20-45, which is associated with active sexual activity, unstable hormone levels and a higher risk of developing gynecological pathologies. In older women, the pathology occurs less often and is associated with a weakened immune system.
Is it possible to cure chronic cystitis?
Like any other chronic disease, cystitis occurs with periods of exacerbation and remission. It is difficult to completely cure the disease, but with the right treatment, you can achieve a stable and very long remission without symptoms from the urinary system.
Do I need a special diet for signs of cystitis?
Yes, during the period of exacerbation of the disease, patients are advised to follow a diet with the exception of salty, spicy, irritating foods. Despite the presence of frequent urination, you should not severely limit your fluid intake. You can drink up to 2 liters of pure water, compote, weak tea. But alcohol and coffee in the acute stage are prohibited.
What features should be considered when choosing a uroseptic?
Let's start with the fact that the choice of the drug and the appointment of an antibiotic regimen is a task only for a specialist: a urologist, a nephrologist, a therapist. It is unacceptable to stop the treatment of cystitis on your own or to change the treatment.
The use of tetracyclines, cephalosporins in cystitis quickly leads to the resistance of pathogens. Therefore, drugs from these groups are practically not used to treat cystitis. Doctors prescribe ampicillins, fluoroquinolones, and various combinations of uroseptic agents. Herbal uroseptics are also widely used, the main advantage of which is good tolerability and the almost complete absence of contraindications. Preparations of this group can be used to treat pregnant and nursing mothers.
The doctor selects a uroseptic individually, analyzing the data of each clinical case. To determine the sensitivity of pathogens to a specific antibiotic, a special study is carried out - bacteriological analysis of urine with inoculation in nutrient media.
How to treat cystitis yourself at home and can it be done?
If symptoms of cystitis appear, it is necessary to consult a urologist, nephrologist or general practitioner as soon as possible. Only a specialist can correctly assess the features of the clinical picture, perform a comprehensive examination, make a correct diagnosis and prescribe the necessary treatment.
But often patients are faced with the fact that a doctor's appointment is scheduled for a certain period of time, and the pain must be relieved right now. To reduce the rate of development of the pathological process, observe the drinking regime - drink about 2 liters of water, compotes, fruit drinks. Hypothermia is a common cause of worsening of the condition, so it is worth dressing warmly and protecting yourself from drafts.
Also try to avoid overexertion. Rest (physical and sexual) will help you wait for an appointment with a specialist. It is undesirable to take analgesics and anticonvulsants on your own without an extreme need - they can "lubricate" the clinical manifestations of the disease, and it will be more difficult for the doctor to make a correct diagnosis.






























